Pressure mounts on B.C.’s health leaders over hospital resource crisis

Posted June 1, 2023 7:28 am.
Last Updated June 1, 2023 10:30 am.
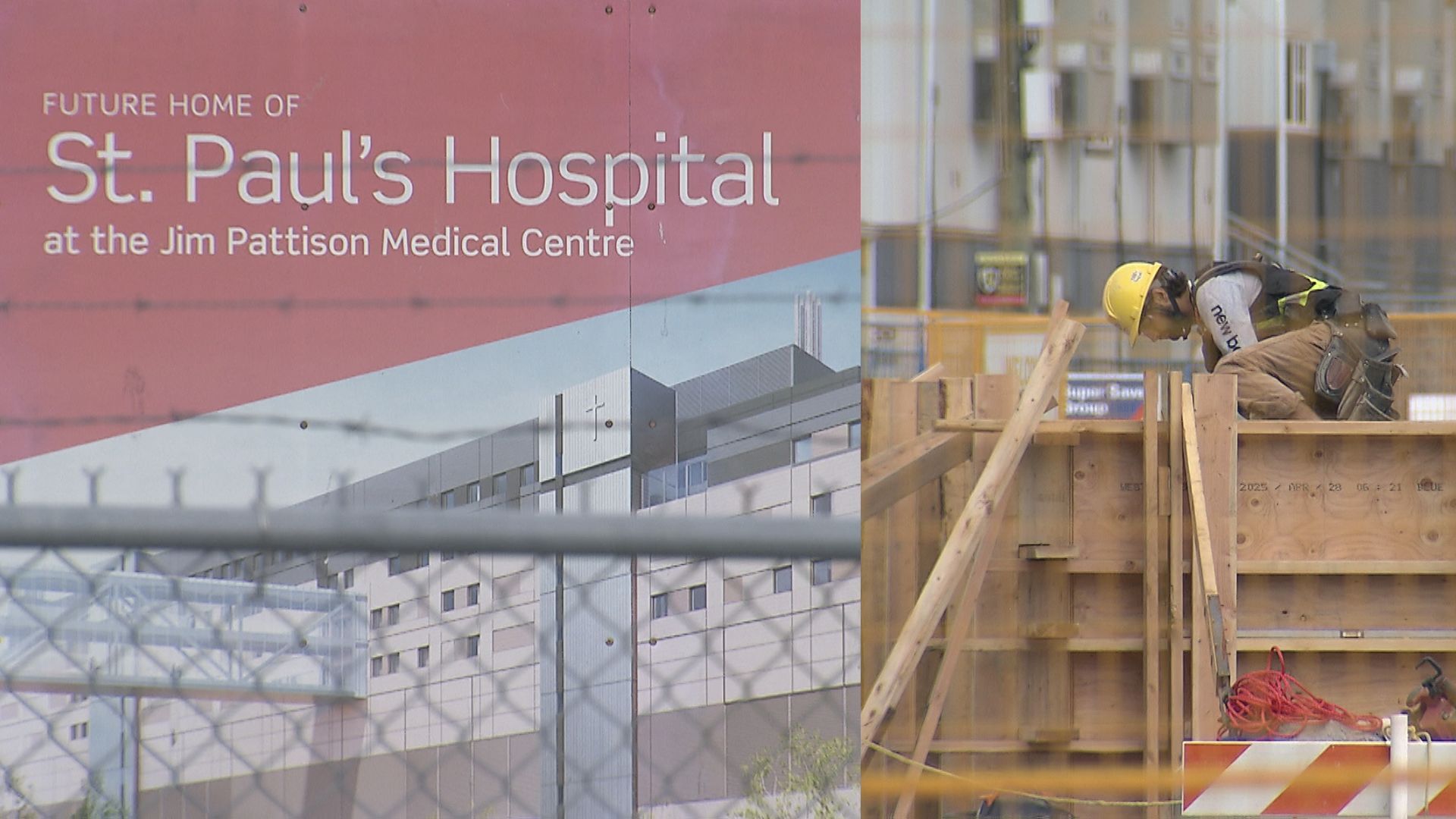
For weeks now, doctors have been speaking out about what they see as a crisis in some of B.C.’s busiest hospitals, with some blaming a critical shortage of resources in hospitals on a lack of leadership in healthcare.
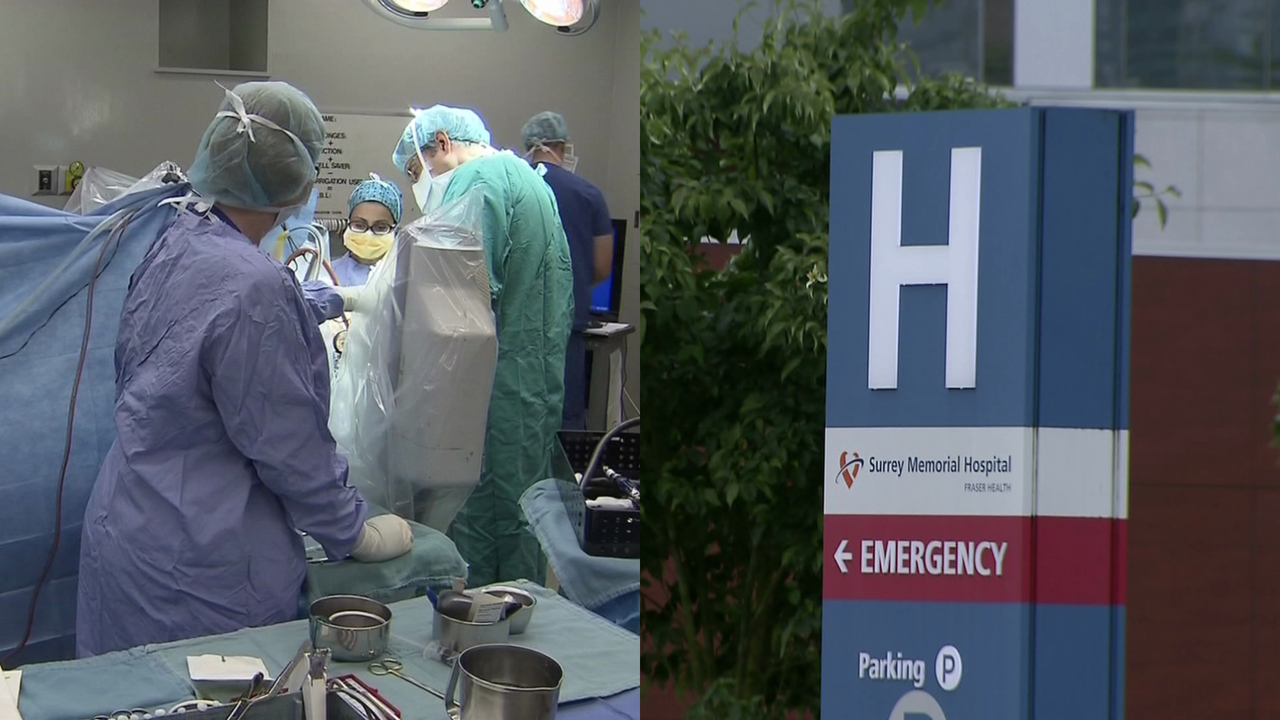
Groups of health providers have been issuing open letters warning about the effects on patient care in facilities like Surrey Memorial Hospital and New Westminster’s Royal Columbian Hospital.
But one of the province’s top doctors suggests there is no quick fix to the problems, and it is not time for heads to roll at the health ministry or health authorities.
“This not any one individual’s problem, this is not one problem that lands on one person’s shoulders,” said Dr. Joshua Greggain, president of Doctors of BC.
“If I can use a sports analogy, the coaches need to assess what’s going on with the players and the players need to be able to speak honestly about what’s happening on the ice. I don’t know that it’s a matter of changing any individual person and whether that would make things any better or worse or different.”
Related Articles:
-
B.C. nurses rally in Vancouver, call on government to address ‘untenable’ conditions
-
B.C. specialist doctors: lack of hospital resources having ripple effect on care
-
Surrey Memorial Hospital crisis: doctors from other hospitals urged to help
Dr. Greggain says when he speaks with health authorities and the provincial health ministry, everyone recognizes there are huge problems in healthcare — the question now, is how quickly a solution can be found.
“The letters absolutely are raising the temperature to say, ‘This is a huge problem and we need to fix it.’ I want to believe that others, including the health minister, the ministry, and the CEOs at the health authorities, genuinely want the system to be better because we are all accountable to the patients we look after,” he told CityNews.
Dr. Greggain points to some recent steps forward, with a one-time $29-million physician funding announcement for the stabilization of in-patient and maternity care in hospitals as well as in long-term care facilities, but some healthcare providers working within the province’s hospitals suggest funding alone can’t fix the problems.
Hospitalists are the backbone of hospitals: doctor
CityNews spoke with a former hospitalist, who wishes to remain anonymous, about B.C.’s shortage of primary care physicians and how it is affecting care in hospitals.
She says the number of general practice doctors has not kept up with the province’s growing and aging population, while the complexity of care for patients has also increased significantly.
The doctor, who is now a locum in the Metro Vancouver region, calls hospitalists the backbone of hospitals like Surrey Memorial and Royal Columbian in the Fraser Health Authority, coordinating complex care for patients, but B.C.’s shortage of primary care physicians has weakened that support.
“Primary care, or general practice, has not been valued over the years.”
“So, over the last 20 or 30 years, resources are put into hospitals and high-level specialists. [But] family physicians — and hospitalists are part of that group — people don’t go into it, or they go into it and don’t like it and they leave it,” she told CityNews.
More recently, she suggests, the agreement between the province and family practice physicians which updated their payment system has made primary care more attractive in B.C., but the result is less incentive to work within the hospital system.
“Family physicians came back to their offices, but there’s a large proportion who were working as half hospitalists, half primary care physicians. When you go back into the longitudinal-family practice program, those benefits are generous,” she said.
“The trouble with being a hospitalist is your team is on 365 days a year, nights, days, evenings, weekends, and holidays. That is an incentive not to do hospitalist medicine if you can do something else.”
She adds greater workloads, the complexity of cases, and an increasing number of hospitalist vacancies are taking their toll.
While hospitalists are in continuing contract negotiations with the province to update things like pay and how many patients they are responsible for, she says hospitalist programs at many facilities have been working at over-capacity for the last few years.
“We have a certain amount of funding to look after a certain amount of patients, but every year that volume keeps going up. You’re being asked to do more and more shifts with constant overtime — that’s the baseline.
“Then when something like the heat dome happens — it still gives me palpitations because we broke all records for numbers of patients coming through the door, we were already over capacity and then we are asked to go up even more.”
She says with many hospitalist shifts now going unfilled, there is chronic pressure to come in during scheduled time off to work extra hours and see extra patients.
“I don’t see a solution for this problem. After the last 18 months, there’s just no one to hire. We used to have, at the hospital I worked at, a position that would open up maybe every year or two and we’d have maybe eight people apply for it. Now programs will have three or four vacant positions and they are lucky if they get one or two applicants. … We are at a point where we simply need bodies and there aren’t any to hire,” she said.
“Could we entice people away from longitudinal family practice back into hospitalist medicine? That’s crazy. We need hospitalists and we need family doctors in the community, so I don’t know how to solve this.”